Tai Chi as a Balance Improvement Exercise for Older Adults a Systematic Review
- Research
- Open Access
- Published:
An evidence map of the effect of Tai Chi on health outcomes
Systematic Reviews book 5, Article number:126 (2016) Cite this commodity
Abstract
Background
This evidence map describes the book and focus of Tai Chi research reporting wellness outcomes. Originally developed as a martial art, Tai Chi is typically taught as a series of ho-hum, low-touch on movements that integrate the jiff, listen, and physical action to achieve greater awareness and a sense of well-being.
Methods
The evidence map is based on a systematic review of systematic reviews. Nosotros searched xi electronic databases from inception to February 2014, screened reviews of reviews, and consulted with topic experts. We used a bubble plot to graphically display clinical topics, literature size, number of reviews, and a broad estimate of effectiveness.
Results
The map is based on 107 systematic reviews. Ii thirds of the reviews were published in the final v years. The topics with the largest number of published randomized controlled trials (RCTs) were general wellness benefits (51 RCTs), psychological well-being (37 RCTs), interventions for older adults (31 RCTs), balance (27 RCTs), hypertension (xviii RCTs), fall prevention (15 RCTs), and cognitive functioning (11 RCTs). The map identified a number of areas with evidence of a potentially positive treatment upshot on patient outcomes, including Tai Chi for hypertension, fall prevention outside of institutions, cognitive functioning, osteoarthritis, low, chronic obstructive pulmonary illness, hurting, rest confidence, and musculus forcefulness. Yet, identified reviews cautioned that firm conclusions cannot be drawn due to methodological limitations in the original studies and/or an insufficient number of existing inquiry studies.
Conclusions
Tai Chi has been practical in diverse clinical areas, and for a number of these, systematic reviews have indicated promising results. The evidence map provides a visual overview of Tai Chi research volume and content.
Systematic review registration
PROSPERO CRD42014009907
Groundwork
Tai Chi, also known every bit T'ai chi ch'uan or Taijiquan, adult as an ancient Chinese martial art and is today widely practiced for its health benefits. Many forms of Tai Chi exist, but in western civilization, information technology is nearly normally taught as a series of slow, gentle, low-impact movements that integrate the breath, mind, and physical activity to achieve greater awareness and a sense of inner peace and well-being. The meditative motion is designed to strengthen and stretch the body, improve the menstruum of blood and other fluids, improve rest, proprioception, and awareness of how the body moves through space; and it may be practiced in a group format or alone [1]. Results from the 2007 National Wellness Interview Survey—a survey of a representative sample of adults in the United states—estimated that approximately ii.3 million adults in the U.s.a. practiced Tai Chi in the past 12 months. There is no official licensure granted by national or state professional boards, and there are no official standards for preparation instructors; thus, individual training programs vary.
Enquiry on effects of Tai Chi on health outcomes continues to expand and has been the subject area of many primary research studies and reviews of the literature. The research field covers a wide spectrum of clinical indications, targets a range of populations, and has focused on a multifariousness of settings. A systematic review of systematic reviews identified 35 reviews published in 2010 and concluded that Tai Chi is effective for fall prevention and improving psychological health and was associated with general health benefits for older people [two]. All the same, the interest in Tai Chi has increased in particular in recent years and since 2010, more than twice every bit many systematic reviews have been published. In order to provide a broad overview of the research evidence that has been published to appointment, we conducted a systematic review of systematic reviews of the effects of Tai Chi on health outcomes [iii].
Nosotros present the results of the systematic review of systematic reviews as an evidence map, a form of systematic literature synthesis that uses visual displays of the volume and content areas of research. Bear witness maps are an emerging show synthesis tool that aim to provide an overview over large inquiry areas [four]. The evidence map presents a summary of the focus of Tai Chi research that contributes to the evidence base on patient health outcomes in a format that is easily attainable to healthcare practitioners and policy makers and other stakeholders. The objective of the show map is to indicate the research focus and bear witness the presence as well as the absence of published inquiry for individual topic areas; the show map may inform research agendas or be used as a signpost for practitioners.
Methods
The testify map is based on a systematic review of systematic reviews and summarizes healthcare inquiry reporting on patient health outcomes on effects of Tai Chi. Systematic reviews provide comprehensive summaries of the literature for divers clinical topics past combining thorough and comprehensive searches and transparent synthesis of the bachelor evidence. Systematic reviews oftentimes employ meta-analysis which provides the statistical ability to place small treatment effects by combining often small and underpowered studies.
We have registered this systematic review in PROSPERO (record number CRD42014009907). We report 1 deviation from the protocol: systematic reviews that do not include randomized controlled trials (RCTs) were not summarized in a narrative synthesis merely were included in the chimera plot in the unclear category of the x-centrality with the y-axis indicating that no RCT was identified despite an explicit search (meet the "Data synthesis" section for more information). This manuscript is based on a comprehensive report for the Department of Veterans Affairs (VA), Veterans Health Administration, Office of Research and Development, Quality Enhancement Research Initiative, conducted within the Evidence-based Synthesis Programme of the VA [iii]. This manuscript aims to disseminate the finding to a broader audience of interested stakeholders. We written report the methodology and results of the evidence map according to the PRISMA guidelines for systematic reviews to the extent possible (the PRISMA checklist is documented in Additional file 1). The VA report discusses the results within the context of the VA healthcare system and includes additional evidence synthesis results for VA-identified priority areas. This evidence map was supported by a technical expert panel of practitioner, policy maker, and researcher content experts.
Data sources
We searched PubMed, CINAHL, Database of Abstracts of Reviews of Effects (Dare), Cochrane Database of Systematic Reviews (CDSR), Health Technology Assessments (HTA), Economic Evaluations (EED), Allied and Complementary Medicine (AMED), PsycINFO, Scopus, Web of Science, and PROSPERO from database inception to February 2014 for published English-linguistic communication systematic reviews. In addition, nosotros screened published reviews of reviews and consulted with topic experts. We used the terms "tai chi," "tai-chi," "tai ji," "tai-ji," "taiji," "t'ai chi," "t' ai chi," "taijiquan," and "shadow boxing;" the total search strategy is documented in Additional file 2.
Inclusion criteria
Design
Systematic reviews focusing on Tai Chi and summarizing principal research studies for all clinical indications were eligible for inclusion. We defined systematic reviews as reviews that either self-identified as a "systematic review" or reviews that reported the search sources and accounted for identified studies.
Participants
Systematic reviews of adult participants or unspecified historic period groups regardless of their health condition were eligible for inclusion in the review; systematic reviews exclusively focusing on children and adolescents were excluded.
Intervention
Systematic reviews of the effects of Tai Chi for whatsoever clinical indication were eligible for inclusion. Systematic reviews addressing Tai Chi and other approaches were eligible if one of the two following criteria was met: (a) "Tai Chi" was part of the search strategy or (b) the search strategy did non specify whatsoever interventions (e.g., focused on an outcome) and the systematic review identified Tai Chi studies. We excluded systematic reviews that included Tai Chi studies but did non systematically search for these (due east.g., by reviewing "exercise" interventions where merely those Tai Chi studies were plant that used the descriptive term "practise") and broad reviews on complementary and culling medicine approaches without particular focus on Tai Chi.
Effect
Systematic reviews reporting on patient health outcomes were eligible for inclusion. Systematic reviews of provider outcomes, credence, prevalence, use, costs, report pattern features, or intervention features not reporting patient health outcomes were excluded.
Timing
Systematic reviews summarizing evaluations of interventions of any elapsing and follow-up point were eligible for inclusion.
Setting
Systematic reviews of studies in healthcare-related settings were eligible for inclusion. English-language systematic reviews, regardless of the linguistic communication of the included studies were eligible for inclusion.
Procedure
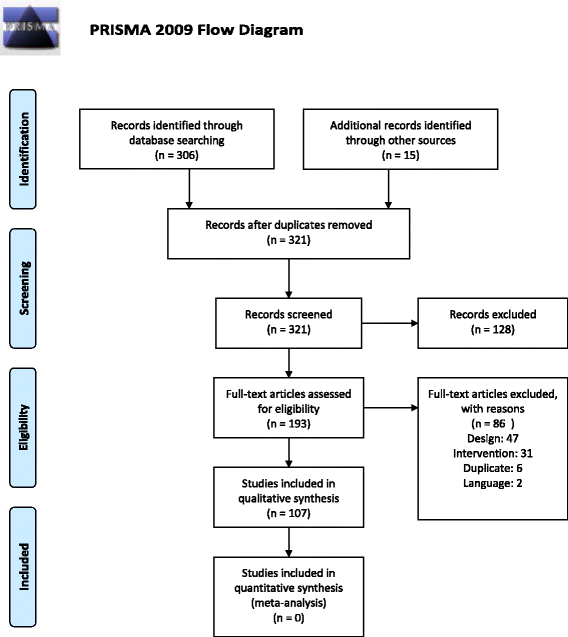
Two independent literature reviewers screened the systematic review search output. Citations deemed potentially relevant past at least one reviewer and unclear citations were obtained as full text. The full-text publications were screened confronting the specified inclusion criteria past two contained reviewers; disagreements were resolved through give-and-take. The reasons for exclusion of full-text publications were recorded (Fig. 1). Where originals and updates of systematic reviews by the same author group were available, only the most recent version was considered, and multiple publications of the same review were counted as one review only information were extracted from all bachelor publications [5–8]. From each included systematic review, we extracted the specific clinical indication (east.g., osteoarthritis) and the main patient outcomes (east.thousand., residuum) that were summarized across included studies. We extracted the number of Tai Chi RCTs included in the review, outcomes measured, comparators, treatment upshot estimates for patient outcomes, and review characteristics. In addition, we documented which reviews were based on a format of Tai Chi that deviated from traditional formats (eastward.g., no weight shifting component; water-based; sitting, non standing; limited training intensity).
Literature flow
Data synthesis
Nosotros used a bubble plot to visually display the Tai Chi research field.
Clinical indications (bubbles)
We used the topics of the identified systematic reviews to categorize the reviews. Reviews focused on outcomes, populations, or clinical indications. Systematic reviews groupings into clinical topics were drafted by one reviewer and discussed in the review team. Decisions non to combine potentially related topic areas (east.g., reviews on the outcome hypertension and reviews on patients with cardiovascular affliction) were based on the lack of overlap betwixt studies included in the reviews, differences in the reported outcomes, and differences in the review'southward conclusion. All identified systematic reviews were allocated to a single content expanse and were merely depicted in one case on the bubble plot.
Color
Indications that have been addressed in a publication by an bureau specializing in unbiased evidence syntheses such every bit Cochrane and the Agency for Healthcare Research and Quality (AHRQ) are shown in nighttime green (all other bubbles are pale yellow).
Number of reviews (bubble size)
We used the size of the bubble to represent the number of systematic reviews on the topic
Literature size judge (y-axis)
The bubble plot provides an overview of the research volume for each of the identified clinical indications. Nosotros used the number of RCTs per review, selecting the systematic review with the most included Tai Chi RCTs for the private topic as the enquiry volume estimate.
Effect guess (x-axis)
The bubble plots provide a very wide indication of the clinical effectiveness of Tai Chi according to patient health outcomes reported in RCTs. All available systematic reviews were reviewed for each clinical indication noted on the evidence map. Greater significance was attributed to the largest review as information technology should provide the nearly consummate literature synthesis, and reviews from agencies specializing in unbiased evidence syntheses as it should provide the well-nigh valid synthesis. Reviews reporting on only ane RCT were classified as unclear evidence regardless of the statistical significance of the private study given the paucity of the existing research and lack of replication of effect. For event size estimates, meta-analytic results were sought to provide a summary effect across individual and oft pocket-sized and underpowered studies. Reviews reporting on studies with alien results across studies were classified as unclear evidence unless they reported a statistically significantly positive pooled effect estimate favoring Tai Chi or all included studies reported a positive effect of Tai Chi. The evidence map is divided into iii sections: topics with prove indicating potentially no event (left department); topics for which the evidence base of operations is unclear (middle section); and topics for which there is published evidence of a potential positive effect with a meta-assay reporting statistically significant treatment furnishings of Tai Chi (correct section).
Results
We identified 321 citations of which 107 unique systematic reviews met the criteria for inclusion in the review [5, 7, 9–113]. Figure 2 provides a graphic representation of the evidence base. 2 thirds (66 %) of the reviews were published in the last five years and spanned a wide diversity of clinical indications, study populations, and outcomes.
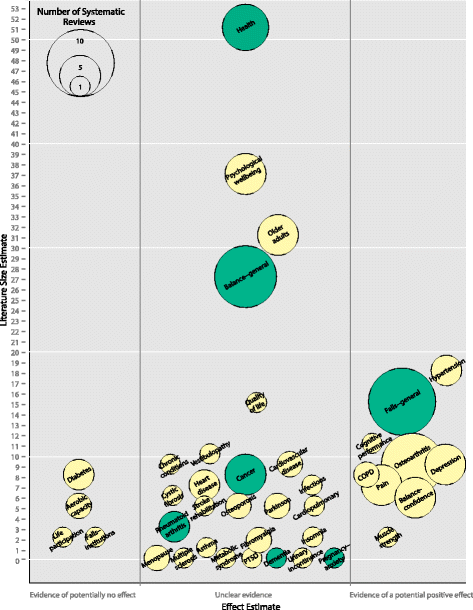
Bear witness map of Tai Chi. The chimera plot displays Tai Chi research based on systematic reviews published to February 2014. y-axis: literature size estimate (number of RCTs included in the largest systematic review). 10-axis: upshot estimate (three partitions: evidence of potentially no effect, unclear evidence base, evidence of a potential positive consequence). Bubbles: clinical indication. Colour: green bubbles indicate that the identified systematic reviews on the topic include a Cochrane review or an AHRQ evidence study. Bubble size: number of systematic reviews on the topic
Size of research base
Topics with the largest enquiry base included research on general health effects, psychological well-beingness, interventions in older adults, and furnishings on the outcome balance, hypertension, falls prevention, and cognitive operation.
The evidence base of operations for the effectiveness of Tai Chi was unclear for the five of the largest areas of enquiry. Half dozen systematic reviews addressed positive effects of Tai Chi on health outcomes (Health) [7, 16, 36, 55, 59, 78]. The largest review, a comprehensive review of health benefits of qigong and Tai Chi, included 51 RCTs simply did not provide treatment effect estimates beyond individual studies [55] and the other reviews primarily highlighted the need for more research. The reviews included studies that addressed a large range of outcomes. The largest review included studies that reported on 163 physiological and psychological health outcomes [55]. An AHRQ evidence report on meditation practices required studies to report measurable information for health-related outcomes and differentiated physiological (due east.g., sensory outcomes), psychosocial (e.g., social and interpersonal relationships), and clinical outcomes (eastward.1000., longevity) [7]. The other reviews differentiated the outcome categories residuum comeback/postural stability/fall prevention, cardiovascular and ventilator enhancement, and other outcomes (rheumatoid arthritis, pain reduction, stress reduction, nightmare reduction); [16] included studies reporting on health outcomes such as cardio respiratory part, falls, rest, forcefulness, or quality of life; [36] reported more than 22 different outcomes addressed in included studies and highlighted furnishings on quality of life, concrete functioning, pain direction, balance and risk of falls reduction, enhancing immune response, and improving flexibility/force/kinesthetic sense; [59] or differentiated effects on cardiovascular disease, chronic disease and amnesty, and psychological benefits [78].
Five systematic reviews concentrated on psychological well-beingness [24, 32, 56, 95, 111]. The largest review included 37 RCTs, but treatment estimates were only presented for iii of the included RCTs [24]. A meta-analysis reported positive pooled results for a few selected outcomes, [95] two reviews did not provide specific handling estimates, [56, 111] and one concluded that it is premature to form conclusions on the effect of Tai Chi on psychological well-being [32]. Four published systematic reviews have examined Tai Chi and qigong for older adults [84, 85, 94, 113]. The review authors focused specifically on this population and did non restrict the reviews to a item clinical outcome. The reviews addressed a range of outcomes and analyses, including perceived benefits to health, perceived improved mediators such every bit social support, and perceived factors for initiating Tai Chi; [84] the efficacy of Tai Chi Chuan based on outcomes reported in included studies such as falls, rest, or cardiorespiratory functions; [94] physical and psychological health outcomes differentiating identified outcomes into the categories falls and residual, physical function, cardiovascular affliction, and psychological and additional disease-specific responses; [85] and validated measures and self-reported indicators of mental well-being such equally life satisfaction, mental wellness-related quality of life, cocky-esteem, or happiness and mastery [113]. The largest review included 31 RCTs; [85] none of the reviews reported specific treatment estimates for Tai Chi across studies.
The event balance has been addressed in nine systematic reviews past independent author groups [10, 37, 39, 53, 57, 61, 72, 77, 109] and the largest review included 27 RCTs. The largest review did not written report treatment effect estimates [57] and an existing Cochrane review on exercise interventions included 12 Tai Chi RCTs but reported furnishings merely for a combination of Tai Chi, gi gong, dance, and yoga interventions [53]. Another review pooled 3 RCTs and found no upshot of Tai Chi on the single leg stance test compared to unlike control groups [10] while results of studies included in the remaining reviews varied and none of the reviews provided a treatment effect estimate across identified studies. A systematic review addressing health-related quality of life included xv Tai Chi RCTs [28] merely did not provide a summary estimate for Tai Chi furnishings and individual study results varied within and across studies.
Potentially promising effects
Promising effects of Tai Chi, indicated by statistically pregnant pooled treatment effects in systematic reviews, and based on a substantial number of enquiry studies included findings for hypertension, falls prevention outside of institutions, and cognitive performance. Hypertension has been addressed in three systematic reviews [68, 97, 106]. The pooled results of the largest review (18 RCTs) showed a larger number of participants with reduced blood force per unit area (relative run a risk [RR] 3.39; 95 % conviction interval [CI] 1.81, vi.34; four RCTs); reduced mean systolic blood pressure level (mmHg WMD 12.43; 95 % CI 12.24, 12.62; ten RCTs); and reduced mean diastolic blood pressure (mmHg WMD 6.03; 95 % CI 5.90, 6.16; 10 RCTs) compared to usual intendance [97]. However, the authors cautioned that the evidence remains weak and stated reservations due to the poor quality of the included studies, lack of longer follow-up, or conflicting results across outcomes, comparators, and settings. An earlier review that included merely 4 RCTs in elderly participants ended that the evidence for Tai Chi in reducing claret pressure level in the elderly is express, [68] and the 3rd review did not provide a pooled handling estimates beyond studies [106]. Tai Chi for fall prevention in unselected populations or participants living in the customs (Falls-full general) has been addressed in 10 independent reviews [17, twenty, 43, 47, 48, 51, 73, 75, 87, 101]. The largest review (15 RCTs) reported no benefit compared to non-exercise controls across 5 studies but found a significant pooled estimate for Tai Chi versus exercise controls (incidence rate ratio [IRR] 0.51; 95 % CI 0.38, 0.68; 2 RCTs); the review discussed a number of explanations for this finding, including a dose-response effect [73]. A Cochrane review on interventions for preventing falls in older people living in the community found no reduction in the rate of falls just reported a significantly reduced risk of falling (RR 0.71; 95 % CI 0.57, 0.87; half dozen RCTs) associated with Tai Chi compared to diverse, predominantly passive comparators (e.one thousand., wellness education) [47]. An AHRQ study on interventions to prevent falls in older adults included 3 Tai Chi RCTs, but no summary treatment effect was reported [twenty]. A further review reported a statistically significant pooled estimate for Tai Chi in customs-dwelling participants (RR 0.66; 95 % CI 0.52, 0.78; comparators not specified) [17]. One review constitute no Tai Chi fall RCTs in older persons with cognitive impairment, and the remaining reviews did not provide a summary effect estimate. Of annotation, reviews in hospitals and nursing dwelling house settings (Falls-institutions) did not study positive findings [nine, 17].
1 systematic review on the furnishings of Tai Chi on cognitive performance in older adults identified 11 relevant RCTs [100]. This review found positive furnishings of Tai Chi on executive part in cognitively good for you adults compared to no intervention (SMD 0.ninety; p = 0.04; 4 RCTs) and exercise (SMD 0.51; p = 0.003; 2 RCTs), on global cognitive office in cognitively dumb adults compared with no intervention (SMD 0.35; p = 0.004; 4 RCTs) or other agile interventions (SMD 0.xxx; p = 0.002; 4 RCTs). Nonetheless, it cautioned that larger and methodologically sound trials with longer follow-up periods are needed before definitive conclusions can be fatigued.
In that location are as well a number of areas suggesting promising results but for which the volume of enquiry is smaller and fewer than ten relevant RCTs were available to inform the reviews. Eight systematic reviews have addressed osteoarthritis [v, 12, 21, thirty, 44, 63, 88, 90, 103], and the two largest reviews included nine RCTs each. One of them reported pooled results and showed positive effects of Tai Chi compared to unlike control groups on hurting (SMD −0.79; 95 % CI −ane.nineteen, −0.39; six RCTs), concrete function (SMD −0.86; 95 % CI −ane.twenty, −0.52; 6 RCTs), and joint stiffness (SMD −0.53; 95 % CI −0.99, −0.08; 6 RCTs) simply cautioned that due to the small number of RCTs with a low adventure of bias, the show that Tai Chi is effective in patients with osteoarthritis is limited [5]. An independent review reported significant positive brusk-term effects for pain intensity (SMD −0.72; 95 % CI −i.00, −0.44; five RCTs), office (SMD −0.72; 95 % CI −1.01, −0.44; 5 RCTs), stiffness (SMD −0.59; 95 % CI −0.99, −0.19; 5 RCTs), and physical quality of life (SMD 0.88; 95 % CI 0.42, 1.34; 2 RCTs) but not for mental quality of life, or long-term effects for pain, concrete part, and stiffness, compared to waitlist or attention control. The authors highlighted that all positive results represent short-term furnishings and high-quality RCTs are needed to ostend the results [63]. A 2013 meta-analysis reported statistically meaning and clinically of import effects for pain (SMD −0.45; 95 % CI −0.seventy, −0.20; 7 RCTs) across studies comparing Tai Chi to waiting listing, Bingo, attention control programs, routine treatment, cocky-assist programs, or wellness education and stretching, and concluded that 12-week Tai Chi programs should be included in rehabilitation programs but highlighted that the pain - relieving effect is not sustained and that additional studies are needed to investigate the long-term effects of Tai Chi in patients with knee osteoarthritis [103]. The remaining reviews did non identify eligible Tai Chi RCTs for their particular review question or did not report handling effects across studies.
Positive outcomes were besides reported in two reviews on chronic obstructive pulmonary disease (COPD) [42, 104] and the largest included 8 RCTs. The largest review reported statistically significant pooled furnishings of Tai Chi for the vi-min walk test (WMD 34.22 m; 95 % CI 21.25, 47.20; 3 RCTs), dyspnea (WMD –0.86; 95 % CI –1.44, –0.28, three RCTs), forced expiratory volume in 1 s (WMD 0.07; 95 % CI 0.02, 0.13, 4 RCTs), forced vital capacity (WMD 0.12; 95 % CI 0.00, 0.23, 3 RCTs), and two quality of life measures (WMD 0.95; 95 % CI 0.22, 1.67; two RCTs; WMD −4.08; 95 % CI −7.52, −0.64; 3 RCTs), comparator not specified [104]. The second review combined Tai Chi and qigong interventions and did not provide treatment estimates across Tai Chi studies. Four systematic reviews have focused on the event hurting [49, 81, 107, 112] and the largest review included seven RCTs (including six arthritis RCTs). The largest review establish a positive effect of Tai Chi on self-reported pain (WMD 10.1 points on a 0–100 calibration; 95 % CI 6.3, 13.9; 6 RCTs; comparators not specified) and self-reported inability (WMD −9.6; 95 % CI −xiv, −5.2; 4 RCTs) but not for physical functioning, and data for quality of life were non pooled beyond studies [49]. Pooled handling estimates of Tai Chi across studies were not reported in two other reviews, and one review found no eligible Tai Chi RCT. Five systematic reviews focused on balance confidence/fear of falling [xv, 18, 33, 83, 91] and the largest included six RCTs. 1 reported a positive effect for Tai Chi compared to usual intendance, practise, or teaching (SMD 0.47; 95 % CI 0.thirty, 0.63; iv RCTs) [83]. The other reviews did not report a treatment result estimate beyond studies. Five systematic reviews have specifically addressed the effects of Tai Chi on depression; [26, 34, 38, 93, 102] the largest review included iv RCTs. It reported statistically significantly reduced depression symptoms (SMD −0.27; 95 % CI −0.52; −0.02; iv RCTs) compared to waitlist in older adults but highlighted that farther enquiry is recommended with larger samples sizes, more clarity on trial pattern and the intervention, longer-term follow-upward, and concomitant economical evaluations [38]. The other depression-specific reviews included only ane or ii Tai Chi studies or did not distinguish effects attributable to Tai Chi. Nonetheless, the review of psychological well-beingness included nine RCTs reporting on depression, and information technology also reported a positive outcome (Hedges' g 0.48; 95 % CI 0.17, 0.78) [95]. A review on lower limb muscle force in the elderly included two RCTs; both reported positive effects but did not report on the same outcome [xi, 114].
Evidence of no effect and unclear or conflicting evidence
The map includes a small number of systematic reviews that provide evidence of the potential lack of effectiveness of Tai Chi for clinical indications beyond more than ane included study, e.g., fall prevention in hospitals and nursing homes (encounter the left hand side of the map). For these topics, systematic review authors ended across identified studies that Tai Chi did not improve outcomes of interest; however, the number of existing studies in the identified topic areas was small in all of the identified topic areas.
In addition, unclear or alien evidence was found for a large number of topical areas as shown in the large middle section of the bear witness map; in some cases, despite a number of existing systematic reviews that have attempted to synthesize the evidence in the enquiry area.
Lack of research
The prove map as well shows clinical topics that have been reviewed, just for which no Tai Chi studies could be found (y-axis = 0). Systematic reviews on menopause, dementia, metabolic syndrome, post-traumatic stress disorder (PTSD), urinary incontinence, multiple sclerosis, and anxiety during pregnancy systematically searched for Tai Chi studies. However, no RCTs, i.e., research studies supporting a high level of evidence, were identified in these systematic reviews.
Other prove base variables
Of the 107 included reviews, 42 % reported on the presence or absence of adverse events (non shown in Fig. 2). The large bulk of these reviews noted that Tai Chi had trivial or no adverse effects on study participants. Nonetheless, doing any practise may put participants at greater risk and one review concluded that Tai Chi practiced past older adults may just be effective in a more robust older population and may not benefit frail participants [48]. None of the included reviews was exclusively based on Tai Chi interventions that deviated from traditional formats.
Give-and-take
This evidence map for Tai Chi is based on 107 published systematic reviews and provides a wide overview of the available evidence of Tai Chi and its upshot on patient outcomes. It shows the research concentration and the volume of available research and highlights areas where published meta-analyses have reported positive results.
Tai Chi has been evaluated for a wide range of clinical applications. Some identified systematic reviews included a big number of RCTs, but they addressed very broad topics such every bit health effects, psychological well-beingness, or interventions targeting older adults. On the other manus, evidence on the role of Tai Chi for a number of specific weather is very limited due to the small number of published studies. Two thirds of identified systematic reviews included in this map were published very recently, i.eastward., in the last five years.
Although testify maps can just provide a broad overview of enquiry areas, it is noteworthy that across clinical topic areas, reviews ended that more rigorous inquiry on the clinical effectiveness of Tai Chi is needed. Furthermore, the effectiveness of Tai Chi may depend on several different factors including setting or patient characteristics—as indicated by differential effects of fall prevention in community versus hospitals or nursing homes. The optimal range of the Tai Chi intervention duration (short term versus long term) has not been determined, and a number of authors have indicated that more research on long-term effects is needed [63].
Our review of reviews also found that agin events of Tai Chi have not been investigated systematically as noted in a recent review [115]. Given that the quality of the reporting of adverse events may depend on the standards in individual clinical fields, analyses across large, multi-indication reviews are particularly useful; a recent review ended that much can exist learned past comparison the effects of a given treatment across many related indications [114].
The evidence map—a visual overview of a systematic review of systematic reviews—is a new and unique review product that shows graphically, at a glance, the volume and focus of a research area through chimera colour, size, and location. Based on a delineated systematic process (east.g., having specified search and inclusion criteria), evidence maps can be used to identify knowledge gaps and future inquiry needs and to provide hands digestible and usable information from a large torso of literature. Because evidence mapping is a relatively new and innovative evidence synthesis method, there are no established reporting guidelines; nonetheless, some principles have been articulated, including the use of an proficient panel to ensure relevance and usefulness of the evidence, such every bit were used in this review [4].
The evidence map has several limitations. First, bear witness maps cannot provide definitive answers nigh the effectiveness of an intervention. We used published reviews to provide an overview over the research on Tai Chi and did not undertake independent systematic reviews to summate effect sizes in a meta-analysis, provide risk of bias assessments, or establish quality of evidence evaluations ourselves. Furthermore, the unit of analysis was systematic reviews, and individual primary research studies will have contributed to more 1 included systematic review, in particular equally reviews focused on different clinical indications, outcomes, or populations. In addition, the group of systematic reviews was review-content driven. The map did not follow a predefined structure and was unable to avoid overlap between included studies beyond reviews; the map was based on published reviews and used the topic structure of the reviews in social club to explore the evidence base of operations. The evidence map used review-level information, not primary research written report data, and relied on the review authors' clinical topic interest and skill in conducting systematic reviews. Furthermore, individual review conclusions may exist limited by the quality of primary studies and susceptible to publication and outcome reporting bias.
Included Tai Chi interventions varied greatly past Tai Chi style, intervention duration, and intervention intensity; and studies varied in their choice of comparator to estimate the effectiveness of Tai Chi. A broad overview cannot answer more refined questions such as the effect of different styles of Tai Chi, the effect of the practitioner's training, and skill level or the function of patients' Tai Chi practice efforts. More specific results demand targeted systematic reviews (addressing selected clinical indications and outcomes) and result modifiers should be analyzed in meta-regressions designed to identify sources of heterogeneity across studies.
Future enquiry should consider the body of evidence assembled in this map and systematically explore the effects of Tai Chi on clinically relevant outcomes across identified reviews. This broad overview has explored the research focus, as described in existing systematic reviews, and the map has identified several promising areas. Establishing more data on the furnishings of Tai Chi across and within clinical indications and patient populations, through meta-analyses across principal research studies, will further advance our evidence-based knowledge of Tai Chi. In addition, the large number of topic areas that were classified as unclear testify warrants farther research. Some topics addressed in reviews were very broad ("health," "psychological well-being," "older adults," or "cancer") and would benefit from targeted syntheses for specific outcomes. In other areas, at that place is a articulate need for boosted primary studies. The lack of positive or negative result estimates is primarily a function of the absenteeism of studies (Tai Chi effects on menopause, multiple sclerosis, metabolic syndrome, PTSD, dementia, urinary incontinence, asthma, and anxiety in pregnancy) at the time of the review. Finally, reviews for some of the topic areas included in the unclear evidence category accept identified an emerging torso of research, but summary effects estimating the treatment effect of Tai Chi are missing and should exist addressed in future meta-analyses.
Conclusions
Tai Chi has been applied in diverse clinical areas, and for a number of these, systematic reviews accept indicated promising results. The evidence map provides a visual overview of Tai Chi enquiry volume and content. Despite the outlined limitations, evidence maps provide valuable data on the landscape—the size, telescopic, and breadth—of a given domain of inquiry. The visualization facilitates an easy and engaging overview and suggests prove maps as a tool useful for a large array of stakeholders and for informing policy and clinical decision makers.
References
-
NIH National Heart for Complementary and Integrative Health (formerly the National Center for Complementary and Culling medicine). Tai Chi: an introduction. 2010.
-
Lee MS, Ernst E. Systematic reviews of t'ai chi: an overview. Br J Sports Med. 2012;46:713–viii.
-
Hempel Southward, Taylor SL, Solloway MR, Miake-Lye IM, Beroes JM, et al. Evidence map of Tai Chi. Washington (DC): Department of Veterans Affairs (Usa); 2014.
-
Hetrick SE, Parker AG, Callahan P, Purcell R. Evidence mapping: illustrating an emerging methodology to amend evidence‐based practice in youth mental health. J Eval Clin Pract. 2010;16:1025–xxx.
-
Kang JW, Lee MS, Posadzki P, Ernst Eastward. T'ai chi for the treatment of osteoarthritis: a systematic review and meta-assay. BMJ Open up. 2011;ane:e000035.
-
Lee MS, Pittler MH, Ernst Due east. Tai chi for osteoarthritis: a systematic review. Clin Rheumatol. 2008;27:211–8.
-
Ospina MB, Bond K, Karkhaneh M, Tjosvold Fifty, Vandermeer B, et al. Meditation practices for health: country of the research. Evidence report/technology cess. 2007. p. 1–263.
-
Ospina MB, Bond K, Karkhaneh K, Buscemi N, Dryden DM, et al. Clinical trials of meditation practices in health care: characteristics and quality. J Altern Complement Med. 2008;14:1199–213.
-
Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2012;ane:CD005465.
-
Leung DP, Chan CK, Tsang HW, Tsang WW, Jones AY. Tai chi as an intervention to ameliorate balance and reduce falls in older adults: a systematic and meta-analytical review. Altern Ther Health Med. 2011;17:40–eight.
-
Liu B, Liu ZH, Zhu HE, Mo JC, Cheng DH. Effects of tai chi on lower-limb myodynamia in the elderly people: a meta-assay. J Tradit Chin Med. 2011;31:141–six.
-
Uthman OA, van der Windt DA, Hashemite kingdom of jordan JL, Dziedzic KS, Healey EL, et al. Practice for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ. 2013;347:f5555.
-
Woods NF, Mitchell ES, Schnall JG, Cray L, Ismail R, et al. Effects of mind-trunk therapies on symptom clusters during the menopausal transition. Climacteric. 2014;17:ten–22.
-
Bo Thousand, Herbert RD. There is not yet strong bear witness that exercise regimens other than pelvic floor muscle grooming can reduce stress urinary incontinence in women: a systematic review. J Physiother. 2013;59:159–68.
-
Bula CJ, Monod S, Hoskovec C, Rochat S. Interventions aiming at balance confidence comeback in older adults: an updated review. Gerontology. 2011;57:276–86.
-
Chen KM, Snyder 1000. A inquiry-based use of Tai Chi/motion therapy every bit a nursing intervention. J Holist Nurs. 1999;17:267–79.
-
Church J, Goodall South, Norman R, Haas K. An economical evaluation of community and residential anile care falls prevention strategies in NSW. Northward S W Public Wellness Balderdash. 2011;22:60–eight.
-
Lach HW, Parsons JL. Impact of fear of falling in long term care: an integrative review. J Am Med Dir Assoc. 2013;14:573–7.
-
Lee MS, Pittler MH, Taylor-Piliae RE, Ernst E. Tai chi for cardiovascular disease and its risk factors: a systematic review. J Hypertens. 2007;25:1974–5.
-
Michael YL, Lin JS, Whitlock EP, Aureate R, Fu R, et al. Interventions to prevent falls in older adults: an updated systematic review. Evidence report no. 80. AHRQ publication no. eleven-05150-EF-1. Rockville: Bureau for Healthcare Research and Quality; 2010.
-
Shengelia R, Parker SJ, Ballin M, George T, Reid MC. Complementary therapies for osteoarthritis: are they effective? Pain Manag Nurs. 2013;14:e274–288.
-
Toh SFM. A systematic review on the effectiveness of Tai Chi exercise in individuals with Parkinson'south disease from 2003 to 2013. Hong Kong J Occup Ther. 2014;23(2):69–81.
-
van der Heijden MMP, van Dooren FEP, Pop VJM, Pouwer F. Effects of exercise grooming on quality of life, symptoms of depression, symptoms of anxiety and emotional well-being in blazon 2 diabetes mellitus: a systematic review. Diabetologia. 2013;56:1210–25.
-
Wang F, Lee EK, Wu T, Benson H, Fricchione Thousand, et al. The effects of Tai Chi on depression, feet, and psychological well-being: a systematic review and meta-analysis. Int J Behav Med. 2013;21(4):605–617.
-
Yan JH, Gu WJ, Pan L. Lack of show on Tai Chi-related furnishings in patients with type 2 diabetes mellitus: a meta-analysis. Exp Clin Endocrinol Diabetes. 2013;121:266–71.
-
Yohannes AM, Caton S. Direction of depression in older people with osteoarthritis: a systematic review. Aging Ment Wellness. 2010;14(6):637–51.
-
Zeng Y, Luo T, Xie H, Huang M, Cheng ASK. Wellness benefits of qigong or tai chi for cancer patients: a systematic review and meta-analyses. Complement Ther Med. 2014;22(one):173–86.
-
Zhang F, Kong LL, Zhang YY, Li SC. Evaluation of impact on wellness-related quality of life and cost effectiveness of Traditional Chinese Medicine: a systematic review of randomized clinical trials. J Altern Complement Med. 2012;18:1108–twenty.
-
Anderson JG, Taylor AG. The metabolic syndrome and mind-trunk therapies: a systematic review. J Nutr Metab. 2011;2011:276419.
-
Escalante Y, Garcia-Hermoso A, Saavedra JM. Effects of exercise on functional aerobic capacity in lower limb osteoarthritis: a systematic review. J Sci Med Sport. 2011;14:190–eight.
-
Marc I, Toureche Northward, Ernst E, Hodnett ED, Blanchet C, et al. Mind-trunk interventions during pregnancy for preventing or treating women'south anxiety. Cochrane Database Syst Rev. 2011;7:CD007559.
-
Wang WC, Zhang AL, Rasmussen B, Lin LW, Dunning T, et al. The effect of Tai Chi on psychosocial well-beingness: a systematic review of randomized controlled trials. J Acupunct Meridian Stud. 2009;ii:171–81.
-
Zijlstra GA, van Haastregt JC, van Rossum E, van Eijk JT, Yardley Fifty, et al. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc. 2007;55:603–fifteen.
-
Determent C, Spanjers K, Patel S, Atherton NM, Lamb SE. Effect of exercise on low severity in older people: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry. 2012;201(iii):180–5.
-
Brown JC, Huedo-Medina TB, Pescatello LS, Pescatello SM, Ferrer RA, Johnson BT. Efficacy of exercise interventions in modulating cancer-related fatigue amongst developed cancer survivors: a meta-analysis. Cancer Epidemiol Biomark Prev. 2011;20(1):123–33.
-
Bu B, Haijun H, Yong L, Chaohui Z, Xiaoyuan Y, et al. Effects of martial arts on health status: a systematic review. J Evid Based Med. 2010;3:205–19.
-
Chan WW, Bartlett DJ. Effectiveness of Tai Chi every bit a therapeutic exercise in improving balance and postural control. Phys Occup Ther Geriatr. 2000;17:i–22.
-
Chi I, Jordan-Marsh Thou, Guo Thou, Xie B, Bai Z. Tai chi and reduction of depressive symptoms for older adults: a meta-analysis of randomized trials. Geriatr Gerontol Int. 2013;xiii:3–12.
-
Conrad Wooton A. An integrative review of Tai Chi research: an alternative class of physical activity to better residue and preclude falls in older adults (Conditional abstract). Orthop Nurs. 2010;29:108-118.
-
Dalusung-Angosta A. The impact of Tai Chi exercise on coronary heart affliction: a systematic review. J Am Acad Nurse Pract. 2011;23:376–81.
-
Ding Yard. Tai Chi for stroke rehabilitation: a focused review. Am J Phys Med Rehabil. 2012;91:1091–6.
-
Ding Grand, Zhang W, Li Thousand, Chen X. Effectiveness of T'ai Chi and Qigong on chronic obstructive pulmonary affliction: a systematic review and meta-analysis. 2013. J Altern Complement Med.
-
El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention do programmes on fall induced injuries in community domicile older adults: systematic review and meta-assay of randomised controlled trials. BMJ. 2013;347:f6234.
-
Escalante Y, Saavedra JM, Garcia-Hermoso A, Silva AJ, Barbosa TM. Concrete exercise and reduction of pain in adults with lower limb osteoarthritis: a systematic review. J Back Musculoskelet Rehabil. 2010;23:175–86.
-
Fairhall N, Sherrington C, Clemson L, Cameron ID. Do practice interventions designed to forestall falls affect participation in life roles? A systematic review and meta-analysis. Age Ageing. 2011;forty(6):666–74.
-
Forbes D, Thiessen EJ, Blake CM, Forbes SC, Forbes S. Practice programs for people with dementia. Cochrane Database Syst Rev. 2013;12:CD006489.
-
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146.
-
Gregory H, Watson MC. The effectiveness of Tai Chi equally a fall prevention intervention for older adults: a systematic review (Structured abstract). Int J Wellness Promot Educ. 2009;47:94-100.
-
Hall A, Maher C, Latimer J, Ferreira M. The effectiveness of Tai Chi for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Arthritis Rheum. 2009;61:717–24.
-
Han A, Robinson V, Judd M, Taixiang W, Wells G, et al. Tai chi for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2004;3:CD004849.
-
Harling A, Simpson JP. A systematic review to determine the effectiveness of Tai Chi in reducing falls and fear of falling in older adults (Structured abstract). Phys Ther Rev. 2008;xiii:237-248.
-
Ho RT, Wang CW, Ng SM, Ho AH, Ziea ET, et al. The result of t'ai chi exercise on immunity and infections: a systematic review of controlled trials. J Altern Complement Med. 2013;19:389–96.
-
Howe TE, Rochester Fifty, Neil F, Skelton DA, Ballinger C. Practice for improving rest in older people. Cochrane Database Syst Rev. 2011;11:CD004963.
-
Innes KE, Selfe TK, Vishnu A. Mind-body therapies for menopausal symptoms: a systematic review. Maturitas. 2010;66:135–49.
-
Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Wellness Promot. 2010;24:e1–e25.
-
Jimenez PJ, Melendez A, Albers U. Psychological effects of Tai Chi Chuan. Curvation Gerontol Geriatr. 2012;55:460–vii.
-
Jimenez-Martin PJ, Melendez-Ortega A, Albers U, Schofield D. A review of Tai Chi Chuan and parameters related to balance. Eur J Integr Med. 2013;5:469–75.
-
Kim SH, Schneider SM, Kravitz L, Mermier C, Burge MR. Mind-trunk practices for posttraumatic stress disorder. J Investig Med. 2013;61:827–34.
-
Klein PJ, Adams WD. Comprehensive therapeutic benefits of Taiji: a critical review. Am J Phys Med Rehabil. 2004;83:735–45.
-
Klein PT, Adams W. Cardiopulmonary physiotherapeutic applications of taiji (Structured abstruse). Cardiopulm Phys Ther. 2004;15:5–11.
-
Komagata S, Newton R. The effectiveness of Tai Chi on improving rest in older adults: an prove-based review (Conditional abstract). J Geriatr Phys Ther. 2003;26:ix–16.
-
Langhorst J, Klose P, Dobos GJ, Bernardy K, Hauser Due west. Efficacy and safety of meditative motility therapies in fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Rheumatol Int. 2013;33:193–207.
-
Lauche R, Langhorst J, Dobos G, Cramer H. A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee. Complement Ther Med. 2013;21:396–406.
-
Lee MS, Choi TY, Ernst East. Tai chi for breast cancer patients: a systematic review. Chest Cancer Res Care for. 2010;120:309–sixteen.
-
Lee MS, Choi TY, Lim HJ, Ernst E. Tai chi for direction of type 2 diabetes mellitus: a systematic review. Chin J Integr Med. 2011;17:789–93.
-
Lee MS, Lam P, Ernst E. Effectiveness of tai chi for Parkinson'due south illness: a critical review. Parkinsonism Relat Disord. 2008;14:589–94.
-
Lee MS, Lee EN, Ernst E. Is tai chi beneficial for improving aerobic capacity? A systematic review. Br J Sports Med. 2009;43:569–73.
-
Lee MS, Lee EN, Kim JI, Ernst Due east. Tai chi for lowering resting blood pressure in the elderly: a systematic review. J Eval Clin Pract. 2010;16:818–24.
-
Lee MS, Pittler MH, Ernst Eastward. Tai chi for rheumatoid arthritis: systematic review. Rheumatology (Oxford). 2007;46:1648–51.
-
Lee MS, Pittler MH, Ernst E. Is Tai Chi an effective offshoot in cancer care? A systematic review of controlled clinical trials. Support Intendance Cancer. 2007;fifteen:597–601.
-
Lee MS, Pittler MH, Shin BC, Ernst E. Tai chi for osteoporosis: a systematic review. Osteoporos Int. 2008;19:139–46.
-
Liu H, Frank A. Tai chi as a residuum improvement exercise for older adults: a systematic review. J Geriatr Phys Ther. 2010;33:103–nine.
-
Logghe IH, Verhagen AP, Rademaker AC, Bierma-Zeinstra SM, van Rossum Due east, et al. The furnishings of Tai Chi on fall prevention, fear of falling and balance in older people: a meta-analysis. Prev Med. 2010;51:222–7.
-
Lorenc AB, Wang Y, Madge SL, Hu X, Mian AM, et al. Meditative movement for respiratory function: a systematic review. Respir Care. 2013;59(3):427–440.
-
Depression S, Ang LW, Goh KS, Chew SK. A systematic review of the effectiveness of Tai Chi on fall reduction amidst the elderly. Arch Gerontol Geriatr. 2009;48:325–31.
-
Macfarlane GJ, Paudyal P, Doherty M, Ernst E, Lewith 1000, et al. A systematic review of evidence for the effectiveness of practitioner-based complementary and alternative therapies in the management of rheumatic diseases: rheumatoid arthritis. Rheumatology (Oxford). 2012;51:1707–13.
-
Maciaszek J, Osinski Due west. The furnishings of Tai Chi on torso balance in elderly people—a review of studies from the early 21st century. Am J Chin Med. 2010;38:219–29.
-
Mansky P, Sannes T, Wallerstedt D, Ge A, Ryan M, et al. Tai chi chuan: heed-body practice or exercise intervention? Studying the benefit for cancer survivors (Structured abstract). Integr Cancer Ther. 2006;5:192-201.
-
Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, et al. Practise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;viii:CD007566.
-
Mist SD, Firestone KA, Jones KD. Complementary and culling do for fibromyalgia: a meta-assay. J Pain Res. 2013;6:247–60.
-
Morone NE, Greco CM. Heed-body interventions for chronic pain in older adults: a structured review. Pain Med. 2007;8:359–75.
-
Ng SM, Wang CW, Ho RT, Ziea TC, He J, et al. Tai chi exercise for patients with eye disease: a systematic review of controlled clinical trials. Altern Ther Health Med. 2012;eighteen:xvi–22.
-
Rand D, Miller WC, Yiu J, Eng JJ. Interventions for addressing depression residue confidence in older adults: a systematic review and meta-analysis. Age Ageing. 2011;twoscore:297–306.
-
Rogers C, Keller C, Larkey LK. Perceived benefits of meditative move in older adults. Geriatr Nurs. 2010;31:37–51.
-
Rogers CE, Larkey LK, Keller C. A review of clinical trials of tai chi and qigong in older adults. West J Nurs Res. 2009;31:245–79.
-
Sarris J, Byrne GJ. A systematic review of insomnia and complementary medicine. Sleep Med Rev. 2011;fifteen:99–106.
-
Schleicher MM, Wedam 50, Wu G. Review of Tai Chi as an effective practice on falls prevention in elderly. Res Sports Med. 2012;20:37–58.
-
Selfe TK, Innes KE. Mind-torso therapies and osteoarthritis of the knee. Curr Rheumatol Rev. 2009;5:204–11.
-
Sharma G, Haider T. Tai chi as an culling and complementary therapy for patients with asthma and chronic obstructive pulmonary disease: a systematic review. J Evid Based Complement Altern Med. 2013;18:209–15.
-
Simic M, Hinman RS, Wrigley Goggle box, Bennell KL, Chase MA. Gait modification strategies for altering medial knee joint joint load: a systematic review. Arthritis Care Res (Hoboken). 2011;63:405–26.
-
Sjosten North, Vaapio S, Kivela SL. The furnishings of fall prevention trials on depressive symptoms and fearfulness of falling among the aged: a systematic review. Aging Ment Health. 2008;12:xxx–46.
-
Taylor-Piliae RE. The effectiveness of Tai Chi exercise in improving aerobic chapters: an updated meta-analysis. Med Sport Sci. 2008;52:40–53.
-
Tsang HW, Chan EP, Cheung WM. Effects of mindful and non-mindful exercises on people with low: a systematic review. Br J Clin Psychol. 2008;47:303–22.
-
Verhagen AP, Immink M, van der Meulen A, Bierma-Zeinstra SM. The efficacy of Tai Chi Chuan in older adults: a systematic review. Fam Pract. 2004;21:107–xiii.
-
Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, et al. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. 2010;ten:23.
-
Wang C, Collet JP, Lau J. The outcome of Tai Chi on health outcomes in patients with chronic weather: a systematic review. Arch Intern Med. 2004;164:493–501.
-
Wang J, Feng B, Yang 10, Liu W, Teng F, et al. Tai chi for essential hypertension. Evid Based Complement Alternat Med. 2013;2013:215254.
-
Wayne PM, Kiel DP, Krebs DE, Davis RB, Savetsky-German J, et al. The effects of Tai Chi on bone mineral density in postmenopausal women: a systematic review. Curvation Phys Med Rehabil. 2007;88:673–fourscore.
-
Wayne PM, Krebs DE, Wolf SL, Gill-Body KM, Scarborough DM, et al. Can Tai Chi better vestibulopathic postural control? Curvation Phys Med Rehabil. 2004;85:142–52.
-
Wayne PM, Walsh JN, Taylor-Piliae RE, Wells RE, Papp KV, et al. Result of Tai Chi on cognitive functioning in older adults: systematic review and meta-analysis. J Am Geriatr Soc. 2014;62(i):25–39.
-
Winter H, Watt K, Peel NM. Falls prevention interventions for community-dwelling older persons with cognitive harm: a systematic review. Int Psychogeriatr. 2013;25(2):215–27.
-
Woltz PC, Chapa DW, Friedmann Eastward, Son H, Akintade B, et al. Effects of interventions on depression in heart failure: a systematic review. Center Lung. 2012;41:469–83.
-
Yan JH, Gu WJ, Sun J, Zhang WX, Li BW, et al. Efficacy of Tai Chi on pain, stiffness and function in patients with osteoarthritis: a meta-analysis. PLoS I. 2013;8:e61672.
-
Yan JH, Guo YZ, Yao HM, Pan L. Effects of Tai Chi in patients with chronic obstructive pulmonary disease: preliminary evidence. PLoS One. 2013;eight:e61806.
-
Yeh GY, Wang C, Wayne PM, Phillips R. Tai chi do for patients with cardiovascular conditions and run a risk factors: a systematic review. J Cardiopulm Rehabil Prev. 2009;29:152–60.
-
Yeh GY, Wang C, Wayne PM, Phillips RS. The effect of tai chi practice on blood pressure: a systematic review. Prev Cardiol. 2008;11:82–9.
-
Reid MC, Papaleontiou G, Ong A, Breckman R, Wethington E, et al. Cocky-direction strategies to reduce pain and amend function amid older adults in community settings: a review of the testify. Pain Med. 2008;nine:409–24.
-
Pan Fifty, Yan J, Guo Y, Yan J. Furnishings of Tai Chi preparation on exercise capacity and quality of life in patients with chronic heart failure: a meta-assay. Eur J Center Fail. 2013;fifteen:316–23.
-
Wu K. Progress in geriatrics Evaluation of the effectiveness of Tai Chi for improving rest and preventing falls in the older population—a review. J Am Geriatr Soc. 2002;50:746–54.
-
Binns EE, Taylor D. Does Tai Chi improve force and residuum in people with multiple sclerosis—the current literature. N Z J Physiother. 2008;36:83.
-
Dechamps A, Lafont L, Bourdel-Marchasson I. Effects of Tai Chi exercises on cocky-efficacy and psychological wellness. Eur Rev Aging Phys Deed. 2007;iv:25–32.
-
Wang XQ, Zheng JJ, Yu ZW, Bi 10, Lou SJ, et al. A meta-assay of core stability practice versus general exercise for chronic low back pain. PLoS I. 2012;seven:e52082.
-
Windle G, Hughes D, Linck P, Russell I, Woods B. Is practise effective in promoting mental well-being in older age? A systematic review. Aging Ment Health. 2010;14:652–69.
-
Chen YF, Hemming K, Chilton PJ, Gupta KK, Altman DG, et al. Scientific hypotheses can exist tested by comparison the effects of one treatment over many diseases in a systematic review. J Clin Epidemiol. 2014;67:1309–nineteen.
-
Wayne PM, Berkowitz DL, Litrownik DE, Buring JE, Yeh GY. What do we really know virtually the rubber of Tai Chi?: a systematic review of agin result reports in randomized trials. Arch Phys Med Rehabil. 2014;95:2470–83.
Acknowledgements
We would like to thank the technical good panel advising on the project: Stephen Ezeji-Okoye, Laura Krejci, Peter Asco, Ansgar Furst, Laura Redwine, Greg Patterson, and Elmer Ligh. We likewise thank Andrew Siroka for assistance with designing the chimera plot, Aneesa Motala for editorial aid, Ning Fu for assistance with the data extraction, and Jeremy Miles for assist with the data synthesis. Any errors of fact or interpretation in this manuscript remain the responsibility of the authors.
Funding
The study is based on a systematic review conducted past the Prove-based Synthesis Programme (ESP) funded by the Department of Veterans Affairs (VA). The funding source deputed the study equally an evidence map but other than that had no function in the behave of the study; collection, management, analysis, and estimation of the data; training, review, or approval of the manuscript; and decision to submit the manuscript for publication. The findings and conclusions in this publication are those of the authors who are responsible for its contents; the findings and conclusions do non necessarily represent the views of the VA or the ESP program.
Availability of data and materials
All included systematic reviews are in the public domain; see the "Reference" section for total citation details. Study flow was tracked in commendation management software and data were extracted in an online systematic review plan and in Excel; all files tin be obtained from the authors.
Authors' contributions
MS and SH drafted the manuscript. SH, PS, and IML designed the study. RS designed and executed the search strategy. JB, IML, MS, SH, and ST were involved in data conquering and assay. All authors were involved in the estimation of the information and contributed to the final manuscript. All authors read and approved the last manuscript.
Competing interests
PS is a Co-Editor in Chief, and SH is an Associate Editor of Systematic Reviews.
Consent for publication
Not applicable
Ethics approving and consent to participate
Not applicative.
Writer information
Affiliations
Corresponding writer
Additional files
Rights and permissions
Open Access This article is distributed under the terms of the Artistic Commons Attribution 4.0 International License (http://creativecommons.org/licenses/past/iv.0/), which permits unrestricted use, distribution, and reproduction in whatsoever medium, provided you give appropriate credit to the original author(south) and the source, provide a link to the Creative Commons license, and betoken if changes were fabricated. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the information made available in this article, unless otherwise stated.
Reprints and Permissions
Nigh this article
Cite this commodity
Solloway, Thou.R., Taylor, S.L., Shekelle, P.G. et al. An evidence map of the effect of Tai Chi on wellness outcomes. Syst Rev 5, 126 (2016). https://doi.org/10.1186/s13643-016-0300-y
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/s13643-016-0300-y
Keywords
- Systematic review
- Tai Chi
- Evidence map
- Health
Source: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0300-y
0 Response to "Tai Chi as a Balance Improvement Exercise for Older Adults a Systematic Review"
Enregistrer un commentaire